Suspected CTE
Treatment Methods
A comprehensive approach that addresses cognitive and physical symptoms.

Focused on addressing your symptoms
There are many therapies available to treat the symptoms associated with suspected Chronic Traumatic Encephalopathy (CTE) that allow patients to have a better quality of life. Under the care of the right doctor, alongside lifestyle changes, most patients will see improvements.
We use the term “suspected” CTE because CTE cannot yet be diagnosed with a known level of statistical accuracy in living patients (learn how you can help advance CTE research by clicking here).
Therefore, treatments are focused on addressing your symptoms, whether they’re from CTE, concussions, or unrelated to your head impact history. We urge you to keep in mind that there is a significant chance you do not have CTE.
When it comes to choosing treatments, there have been very few scientific studies on how to treat the clinical symptoms of CTE and even fewer clinical trials exploring innovative therapies that could slow or stop the progression of the disease.
While CLF works to grow the interest and infrastructure in CTE clinical trials, we’re here to tell you what’s working today, and how you can start to feel and live better.
Learn from clinicians who specialize
in treating suspected CTE
In 2019, Concussion Legacy Foundation co-founder and medical director Dr. Robert Cantu and Andrew Budson, Associate Director
for Research at the Boston University Alzheimer’s Disease Center, published the first ever CTE management recommendations in
Expert Review of Neurotherapeutics.
The review is meant to assist clinicians in diagnosing CTE as unlikely, possible, or probable and suggests both nonpharmacologic
and pharmacologic treatments for symptoms of CTE in order to help improve quality of life. You can view or download the abstract
here to share with your doctor.
Dr. Robert Cantu’s approach to treating patients with suspected CTE
Criteria for identifying CTE
Diagnosis of CTE
Management of CTE symptoms
Pharmacological treatments
Criteria for identifying CTE
Diagnosis of CTE
Management of CTE symptoms
Pharmacological treatments
Criteria for identifying CTE
When treating suspected CTE symptoms, a clinician’s first step is to understand your exposure to repeated traumatic brain injuries and repetitive head impacts. More than 90% of individuals diagnosed with CTE experience repetitive head impacts through regular participation in contact sports and/or military service. Studies of deceased American football players suggest that CTE is unlikely if an individual has not played for five years or more. Data is not yet available on other sports.
While CTE cannot be definitively diagnosed during life, experts led by the Boston University CTE Center are developing criteria for diagnosing Traumatic Encephalopathy Syndrome (TES), which is designed to capture the symptoms caused by CTE during life. Unfortunately, TES criteria are still limited to research studies, and not yet used by doctors.
Diagnosis of CTE
Currently, the presence of CTE can only be established through a neuropathological examination after death. Research is ongoing to find biomarkers in the blood, as well as imaging techniques, that might allow for an earlier definitive diagnosis.
Clinicians currently rely on the patient’s clinical history and symptom presentation to establish a presumptive diagnosis. The process involves detailed interviews with the patient, and often family members, to piece together the history of head trauma and the timeline of symptom development.
Neurological examinations, cognitive tests, and functional capacity assessments can also help inform CTE’s likelihood.
Management of CTE symptoms
The management of CTE symptoms requires a comprehensive approach that addresses both physical and cognitive symptoms. Individualized care plans focus on improving the quality of life for those affected, while cognitive therapies help improve functioning and assist individuals in adapting to their limitations.
Behavioral therapies have been proven to address the emotional and psychological challenges of suspected CTE, providing techniques to cope with mood swings, depression, and potential aggression.
Physical therapy also plays a pivotal role in managing motor symptoms, helping to preserve mobility and function.
Pharmacological treatments
According to Dr. Cantu, the pharmacological factors for managing CTE include a range of medications, each targeting specific symptom clusters.
- Cognitive enhancers: Medications like Aricept (donepezil) and Namenda (memantine) are used to mitigate memory loss and confusion.
- Antidepressants: These medications play a key role in managing the complex emotional landscape of suspected CTE, from lifting the fog of depression to curbing rage and anxiety.
- Mood stabilizers: Used to smooth the ups and downs of emotional volatility, mood stabilizers can make a big difference in the lives of those with suspected CTE experiencing bipolar-like symptoms.
- Sleep: Melatonin and other sleep aids are sometimes prescribed to combat the sleep disturbances commonly reported in suspected CTE cases, aiding in a more restful sleep cycle.
Dr. James Castle’s insights on managing and treating CTE
Demographic variations in CTE symptoms
Suspected CTE treatment approaches for younger patients
Demographic variations in CTE symptoms
Suspected CTE treatment approaches for younger patients
Demographic variations in CTE symptoms
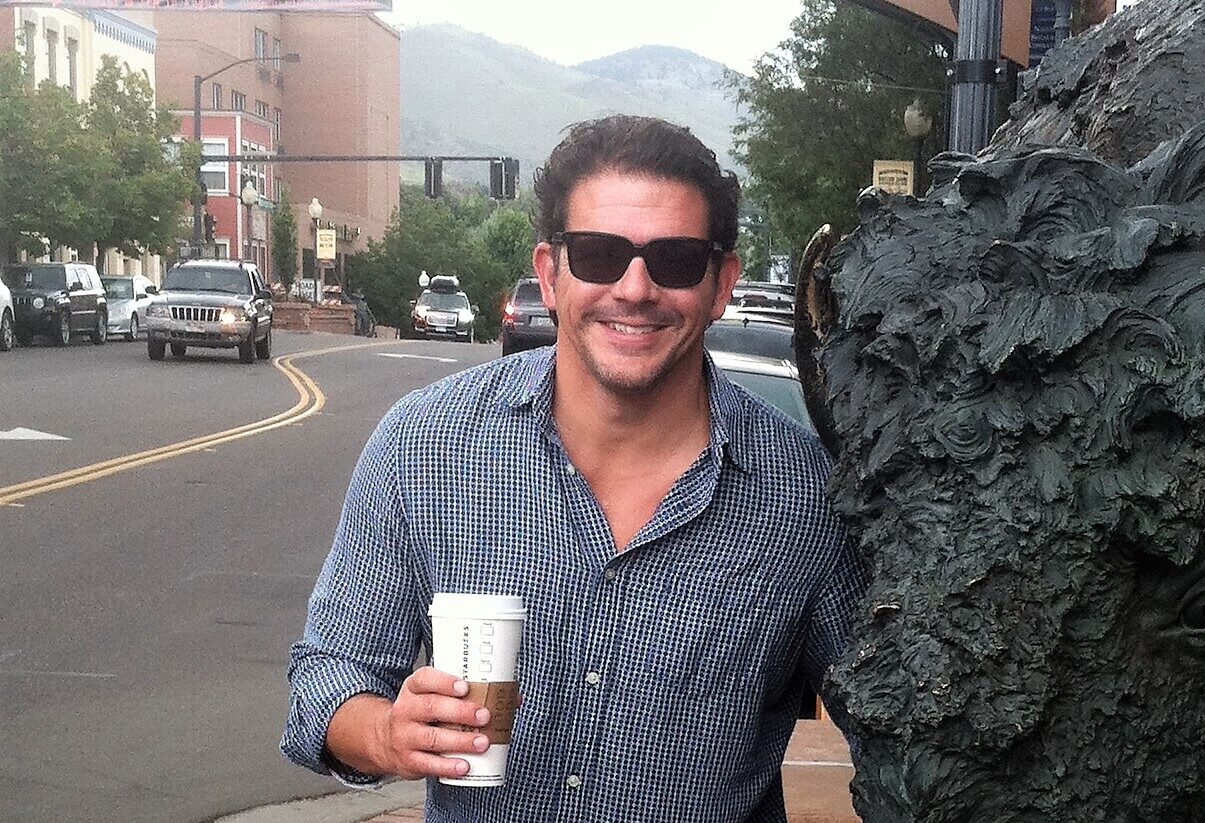
Dr. James Castle is a Cognitive and Behavioral Neurologist at Rush University Medical Center who grew up on the football field from childhood through college. His personal experience with CTE, even before it was a known entity, began with the death of two teammates, one later confirmed to have CTE.
Heavily influenced by his personal connections and his own athletic history, he has made it his mission to observe and treat suspected CTE. One key component of his work has been identifying how suspected CTE presents differently across various age groups.
Younger suspected CTE patients
Younger individuals often encounter a cluster of behavioral issues, including anxiety, depression, rage, and sleep disturbances. Their cognitive challenges primarily involve short-term memory loss and difficulty in executive functions, which disrupt their daily living and normal activities.
Experts now believe that these symptoms are not primarily driven by CTE in most cases, if CTE is present at all. Instead, these symptoms are more likely to be related to suffering multiple concussions, or they could be unrelated to head impact history. That means these symptoms are not progressive and they should be treatable.
Older suspected CTE patients
Older patients often present with progressive cognitive impairments similar to Alzheimer’s disease, with pronounced memory deficits and a decline in cognitive abilities over time. These symptoms can pose significant complications in diagnosis, as they closely mimic other neurodegenerative conditions.
Suspected CTE treatment approaches for younger patients
Dr. Castle promotes a comprehensive care strategy for younger individuals dealing with suspected CTE:
Lifestyle as CTE treatment
Lifestyle choices have a significant impact on brain health and overall well-being.
- Regular physical activity: Following a structured exercise routine that not only aids in maintaining physical fitness but has also been shown to improve mood and cognitive function. Aerobic exercises, strength training, and yoga can play a vital role in neuroprotection and neurodegeneration.
- Cognitive engagement: Taking part in activities that stimulate the mind, such as puzzles, reading, learning new skills, or engaging in any form of creativity can improve neural pathways and potentially slow the progression of symptoms.
- Diet: Due to its anti-inflammatory properties, the Mediterranean Diet has been shown in research to be effective in maintaining brain health. The Mediterranean Diet emphasizes plant-based foods and protein with healthy fats, with very little red meat consumption.
- Weight loss: Many former athletes have reported symptom improvement after weight loss. Being overweight can contribute to chronic pain, limit one’s ability to exercise, and can impact sleep.
Importance of sleep
The link between sleep and cognitive health has been clearly established. Measures you can take to optimize your sleep include:
- A regular sleep schedule: Go to bed and wake up on a consistent schedule every day to regulate circadian rhythm.
- Optimal sleep environment: Create a relaxing sleeping environment that is dark, quiet, and cool.
- Relaxation techniques: Meditation, deep breathing exercises, or progressive muscle relaxation before bedtime can also reduce anxiety and promote restful sleep.
- Sleep study: Having a muscular neck or a history of concussion are risk factors for sleep apnea and other sleep disorders. If you mention these concerns to your doctor, they may recommend a sleep study and treatment that could change your life.
How to find the right doctor
When searching for a specialist to help treat suspected CTE, look for a clinician who specializes in evaluating and treating brain disorders involving cognitive, mood, and behavioural difficulties. This doctor may be a neurologist (especially a cognitive or behavioural neurologist), a psychologist (especially a neuropsychologist), or a psychiatrist (especially a neuropsychiatrist).
Since CTE is a neurodegenerative disease, a clinician who specializes predominantly in concussions or traumatic brain injury may not be appropriate. Rather, a clinician who understands disorders such as Alzheimer’s disease, frontotemporal dementia, and related conditions may be the better choice.
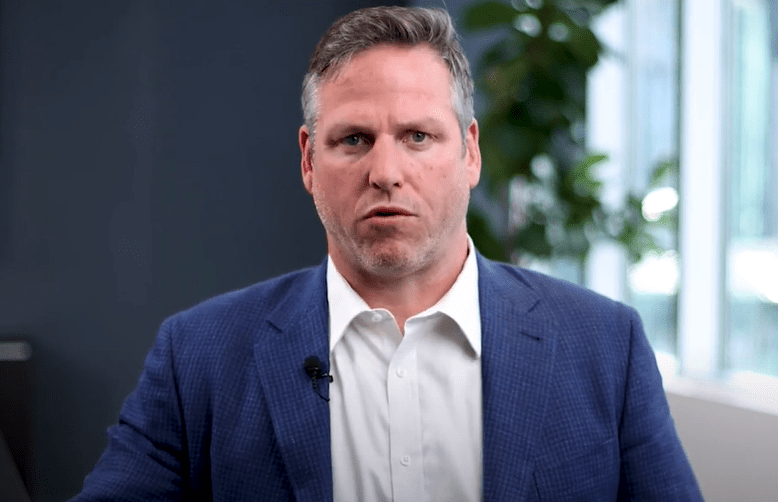
To learn about which type of doctor to see for suspected CTE, and what to discuss with your doctor, watch this video featuring Tim Fleiszer, Executive Director of CLF Canada.
If you’re concerned about, or living with, suspected CTE and are struggling to find the right doctor, please reach out to the CLF HelpLine.