Did Football Kill Austin Trenum?

When a well-adjusted Virginia teen suddenly killed himself, his parents looked for warning signs they had missed. But Austin had no dark secret, no teen angst. There was nothing—except for a concussion he had sustained during a football game a few days earlier.
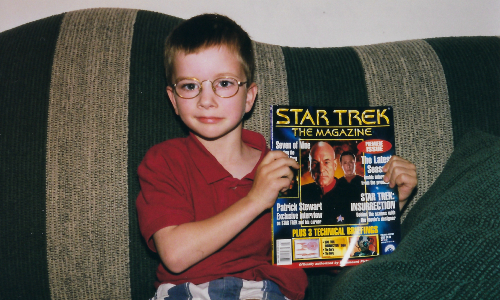
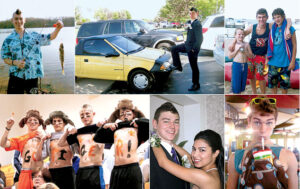
On the day he took his own life, Austin Trenum ate cheesecake. He was 17. He loved cheesecake. He loved the Beastie Boys, too, and SpongeBob Squarepants and the silly fauxhawk haircut he spent months cultivating and two minutes shaving off because, well, that’s what teenagers do. He loved his little Geo Metro convertible, neon yellow and as macho as a golf cart, a gift from his grandfather, the two driving all the way from Texas to Austin’s home in Nokesville, Virginia, a close-knit
community of 1,354 in Prince William County.
Austin loved his parents, Gil and Michelle, and his younger brothers, Cody and Walker. He loved his girlfriend, Lauren. He loved cheering for the girls’ volleyball team at Brentsville District High School, smearing his chest with paint and screaming his lungs out alongside his lacrosse teammates; loved sneaking out of his chemistry class to sing “Bohemian Rhapsody” with his friend Carmen in the band room; loved fishing and paintball, roller coasters and blasting “Sweet Caroline”
with the top down.
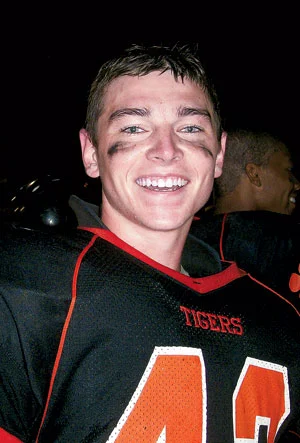
He especially loved football. Loved watching the Dallas Cowboys. Loved playing for the Brentsville varsity team—fullback and linebacker—taking hits and delivering them, seldom leaving the field, eating two Hostess cherry pies before every game. He was a handsome kid, green-eyed like his mother, six feet tall and 190 pounds, growing stronger and more confident all the time. Under the Friday-night lights, in his beat-up helmet and shoulder pads, you could see the man Gilbert Allen Austin Trenum III was becoming.
• • •
It was Sunday, September 26, 2010. Michelle Trenum woke up around 8 am. Gil was out of town, returning that afternoon from a weekend drill with his Navy Reserve unit in New Jersey. Walker, ten, their youngest, was on the living-room couch, hiding under a blanket. He jumped up when Michelle walked in. Boo!
“Austin’s awake,” Walker said. “He’s in the basement playing a video game.”
That’s odd, Michelle thought. Austin never got up early on Sundays. Not voluntarily.
Michelle made her sons breakfast. Austin drove his other brother, Cody, 15, to a lacrosse game and cheered from the sidelines. He took more pride in his siblings than himself; he was that kind of brother. On the way home, he teased Cody. “You did good,” Austin said, before delivering the punch line. “You surprised me!”
Back at the house, Austin ate lunch. And cheesecake. While Austin surfed the Internet, he and Michelle talked about Adam James, a Texas Tech football player who had allegedly been locked in a dark electrical closet by the school’s head coach, Mike Leach, after suffering a concussion. The story, which ultimately ignited a media firestorm and led to Leach’s firing, began when the injured James showed up to practice in sunglasses and street clothes; Austin joked with his mother that he should do the same, just to see how his high-school coach, Dean Reedy, would react.
Austin then turned serious, balancing on one foot to mimic a neurological test.
“Am I going to be out all week?” he said. “I don’t want to be out all week. Do you think I’ll be out two weeks?”
“You’ll just have to see,” Michelle said.
During a football game the previous Friday night, Austin had sustained a concussion. Brain trauma had been in the news. There were reports of retired NFL players suffering from depression and dementia linked to their hard-hitting careers. There were congressional hearings, some of them dealing with high-school football. In the coming months, the sport would be engulfed in a full-blown health crisis. Austin’s parents were mostly unaware of the controversy. They had both grown up in Texas,
where football was king, where getting your bell rung was just a part of the game. Almost a badge of honor.
• • •
Gil and Michelle had been in the Brentsville High bleachers on Friday night, chatting with friends, a full moon overhead. Neither of them saw the hit, but Gil spotted their son standing with his helmet off, touching his index finger to his nose at the direction of team trainer Richard Scavongelli. Just like last season. Good grief.
On the sideline, Austin was dazed, slurring his words. During the drive to the emergency room, he was alert enough to call Lauren, his girlfriend. By the time he was standing in line at Prince William Hospital, shirtless and sweaty, he seemed fine. He cracked jokes, flirted with the nurses who brought him a sandwich and a soda. He begged a doctor to let him leave, asked if Lauren could come back to the examination room.
A nurse asked if he wanted Tylenol.
“The last time you got a concussion, you got a headache,”
Michelle said. “Are you sure you don’t want it?”
“Mom, I’m fine,” Austin said. “I don’t have a headache. Except
for my normal football headache. I get them after every game.”
The medical staff gave Gil and Michelle a sheet of instructions: Watch for vomiting and clear fluid coming out of Austin’s nose, signs of a more severe brain injury. Limit their son to “quiet activities” for the next 24 hours. Wake him from sleep every few hours to check for evidence of intracranial bleeding, such as confusion and extreme
drowsiness.
Heading home, the Trenums stopped at the Chuck Wagon, a restaurant around the corner from their house, where the Brentsville High players gathered after games. Austin’s teammates recounted his sideline exchange with Scavongelli.
Scavongelli: “Do you know where you are?”
Austin: “Yeah. This is my field!”
Scavongelli: “No. Do you know what school you are at?”
Austin: “Yeah. My school!”
Scavongelli: “Do you know who you’re playing against?”
Austin: “No.”
This is my field! Everyone laughed. They laughed at the way Austin had gotten emotional on the field, too, cussing out one of his buddies, something he never, ever did.
On Saturday morning, Austin attended football film study; that afternoon, he went fishing; in the evening, he took Lauren to a Sugarland concert, a belated celebration of her birthday. They sat on the Jiffy Lube Live lawn, taking pictures under the stars. When Austin got home, he texted Lauren good night. The next day, he was sitting in his family’s dining room doing homework, texting her again about meeting up two hours later to watch a Redskins game.
Austin was a good student, ranking in the top 6 percent of his class. He planned to study chemical engineering in college and was deciding between Virginia Tech and James Madison. The former had a better football team; the latter, he deduced during a campus visit, had better-looking girls. As Austin studied for his Cold War history class, Michelle went online to check his academic progress. There was a problem. He hadn’t turned in two papers. Michelle was upset and lectured him about slacking off.
Gil came home around 2:30 pm. Michelle gave her husband a kiss and cut him a slice of cheesecake. She told him about Austin’s schoolwork. Austin looked irritated—almost angry. That was out of character. Michelle saw his jaw clench. His mouth moved. She was stunned. Did he just call me a name? Austin stared straight ahead.
“If you don’t finish your work,” she said, “you can’t see Lauren tonight.”
Gil and Michelle went outside. Cody and Walker were on the living-room couch, watching a football game. At some point, Austin went upstairs.
“I don’t know what’s wrong with Austin,” Michelle said. “He shouldn’t disrespect me like that.”
“He’s a teenager,” Gil said. “I’ll go talk to him.”
Gil went inside. He passed the kitchen table, where his cheesecake sat untouched. He walked up the stairs, the same stairs where Austin would ambush Walker when he came home from school, peppering him with foam darts from a toy gun. The door to Austin’s room was open.
Michelle Trenum heard her husband scream.
• • •
On her way to the hospital, Patti McKay made a deal with God. Not Austin. Please. Take me instead. The boy was like a second son. Every summer, the McKay and Trenum families vacationed together at a lake in Maine, where the kids would play King of the Dock—wrestling for control of a wooden swimming platform, tossing one another in the water, Austin always making sure the younger children won their share.
When her cell phone rang, Patti was in her sister’s garden, kneeling in the dirt. It was Cody, panicked. Austin wasn’t breathing. Gil was trying to resuscitate him. An ambulance was on the way. What should they do?
Keep performing CPR, Patti said.
A cardiology nurse, Patti suspected a subdural hematoma. A brain bleed. Which was odd. She had just seen Austin, about 90 minutes earlier, pulling up in her driveway—the top down on his little yellow convertible, Cody in the passenger seat.
Austin had been grinning. He had a gift with him, a Snickers cheesecake.
“Here, Ms. McKay,” he said. “Look what we brought for you.”
“How are you feeling?”
“Okay.”
“No, really—how are you feeling?”
“I’m fine. My headache is almost gone.”
Patti had been at the game on Friday night, standing with Austin in the Brentsville High parking lot, holding his arm to help him balance. But today his gait was normal, his hands weren’t shaking. She called the emergency room, professional instincts taking over. You’re getting a boy who had a concussion two days ago. You need a neurosurgeon. If you don’t have one, have a helicopter ready to evacuate. Arriving at Prince William Hospital, she didn’t see a helicopter. She saw Rob Place, the Trenums’ next-door neighbor.
Austin hanged himself, Place said.
• • •
Nothing made sense. Not suicide. Not Austin. Not the boy who went deer hunting in West Virginia with his father and crafted elaborate zombie-apocalypse defense plans with Walker. Not the young man who always said “Yes, sir” and “No, ma’am” and was adored by his friends’ parents. Not the charmed kid who never got mad on the lacrosse field, who’d scored a goal six seconds into his first high-school game.
“If someone came to me and asked me to rank, 1 to 25, the kids on the team most likely to have problems and the kids who were the most stable, Austin was number one on the stable end of the list,” says Carl Kielbasa, Austin and Cody’s former high-school lacrosse coach. “His maturity level was extremely high. Never experimenting with drugs and alcohol. Almost fatherly to his brothers. Had a wonderful sense of humor. He was a great teammate, very attentive and aware, very patient and kind. A big-time leader on the team and in school—he could hang out with the kids who were partyers and be in an honor-society meeting the next day. Everyone loved him.”
Austin was taken to Inova Fairfax Hospital, where he died at 2 am on Monday. The entire community was stunned. The boy was beloved. Football was beloved. In the Nokesville area, plans were underway to build a new $850,000 youth-football complex; elementary-school students were let out early on Friday afternoons, the better to high-five Brentsville High players as they made their march down the town’s main road.
How could this have happened?
The Trenums went home. Later that day, their phone rang. Laura O’Neal answered. She was Austin’s godmother, one of Michelle’s best friends. She’d been there for Austin’s first birthday, eating cowboy-themed cake; there when he got his first lacrosse stick, which he carried everywhere, like a scepter. Now she would plan his funeral.
There was a man on the line, Chris Nowinski, a former Harvard football player, calling on behalf of scientists at Boston University.
They wanted Austin’s brain.

The human brain is a wondrous thing. It enables us to throw a football, allows us to breathe, think, and love. In its neurons and glial cells, synapses and neurotransmitters, it is essentially who we are.
And who we are is fragile.
Gerard Gioia opens his laptop. On the screen is a video depicting a brain inside a skull. The brain, he explains, is a spongy mass of tissue. Surrounded by fluid, it moves independent of the skull, just slightly, the arrangement providing a protective measure of shock absorption.
“And this,” he says, “is why the helmet will never be the simple answer to this injury.”
Helmets prevent skull fractures but not concussions. Gioia clicks a button. The head rocks back and forth. The brain smashes against the inside of the skull. The screen flashes like a strobe light, a comic-book pow! Such is the basic dynamic of a concussion, an injury that occurs in football with alarming regularity: According to the American Association of Neurological Surgeons, 4 percent to 20 percent of high-school and college players will suffer one during a single season. That’s likely a low estimate—some experts believe as many as eight of ten concussions go undiagnosed.
“When the head or the body takes force, the brain moves,” explains Gioia, head of Pediatric Neuropsychology at Children’s National Medical Center and an expert on youth and adolescent sports concussions. “It has a certain threshold, beyond which it stretches and strains.”
Gioia loves football—played it himself in high school and college. He wants to make the sport safer. Three weeks after Austin’s death, he met with Gil and Michelle in his Rockville office, where a New York Giants-themed street sign hangs on the wall. Michelle brought a picture frame containing three photos of Austin, including one of him
joyfully painting his face before a volleyball game the week before his death.
“Look at this boy,” she said, fighting tears. “Look at these pictures. He wasn’t depressed.”
Shock giving way to despair, the Trenums wracked their brains. Was there something we missed? They talked to Austin’s friends, checked his text messages, read the journal he kept for English class: I heard my favorite Sublime song. Today was good. I forgot to wear my Hawaiian shirt. Bummer.
No angst. No suicide note. No sign that anything was wrong. Nothing. The concussion, they figured—it had to be the concussion. But how? Didn’t they go to the ER, keep Austin from strenuous activity, do everything right? Scavongelli, the Brentsville High trainer, had immediately pulled Austin from the game, protecting him from second-impact syndrome, a rare but horrific condition in which athletes suffer a second concussion while recovering from a previous one, causing rapid, catastrophic brain swelling that ends in severe disability or death.
After a concussion during his junior year, Austin was held out of football practice for a week. A medical-hotline operator advised Michelle to watch for signs of depression. She told Austin. He laughed.
Oh, please, Mom.
“Why?” says Michelle. “Why did he do this? We must have said that seven million times.”
• • •
A concussion is not a bruise. It’s a disruption of the intricate system of electrochemical signals that constitute normal brain function. Contrary to widespread belief, concussions don’t always coincide with loss of consciousness. Symptoms include headaches, sensitivity to light, confusion, lack of focus, irritability, and loss of interest in
favorite activities.
With rest and a gradual return to regular activity, most athletes who suffer a single concussion experience no permanent ill effects. Some, however, suffer post-concussion syndrome, in which symptoms persist for months or years, in rare cases permanently. Having one concussion may increase the risk of another. Multiple concussions are
associated with an increased risk of post-concussion syndrome as well as depression and memory loss.
Think of your brain as a computer, Gioia says. The tissue is the hardware, and the electrochemical signals are the software. Concussions can scramble both, disrupting healthy equilibrium. Moreover, they leave the brain drained of energy, like a cell phone with a bad battery.
The best treatment? Rest—lots of it. Waking a sleeping concussion patient every few hours to check for brain bleeding has long been conventional medical wisdom, Gioia says, but actually is not a good idea: You should check on them, but not disrupt their sleep. “The essential aspect is allowing the cells to rebalance themselves. Overworking the brain interferes with that recovery. And it’s not just avoiding additional blows to the head. You can’t be out running. You need good sleep. You have to manage school, any activity that involves a lot of thinking.”
• • •
For 21/2 hours, Gioia and the Trenums talked, going over Austin’s final weekend. As they connected the dots, two things became clear: Football had injured his brain, which subsequently was overworked. Texting. Video games. Driving. Studying. Staying up late. Normal teenage activities. All of them too much.
Looking back over the weekend, they saw warning signs, subtle indicators that something was amiss. Austin had trouble sleeping on Sunday morning. He got lost on the way to Cody’s lacrosse game, even though the directions consisted of a single right turn. He forgot what month it was while fishing with his friend Carmen. He had “football headaches.”
When Austin was concussed a few plays before halftime during a football game his junior year, his teammates were the first to notice. In the locker room, he couldn’t figure out how to work his chin strap and began to bawl. Similarly, his final concussion left him cursing out his best friend, Ryan Hall, for an on-field prank meant to make Austin
laugh.
Gioia showed the Trenums a diagram of the brain. He pointed out the frontal lobes, about one-third of the total brain mass, the portion just behind the forehead, where so much football contact takes place. These gelatinous hunks of meat, he told them, are our executive control centers. They allow us to reason, to choose right from wrong, to override impulses, to connect current actions to future consequences.
In teenagers, the frontal lobes are still developing; in everyone, they require a great amount of energy to function properly. Damage or disrupt them, stretch them like Silly Putty, and concentration suffers. Memory gets spotty. The systems governing emotion and reason are thrown out of whack. You might forget how to work a chin strap; you might consider that unbearably tragic. Nothing makes sense.
Austin’s parents believe that their son may have suffered as many as four concussions during three years of playing football. Did those injuries lead him to take his life? Gioia can’t say. There’s no direct causation. The brain remains mysterious.
“My thought to the Trenums was that Austin’s brain wasn’t functioning properly,” he says. “It was drained in terms of overall energy, unusual emotional response was one of his manifestations, and the argument about academics hit at that time. Bam! Those emotions go off, and now the decision-making is not working properly, either.”
Meeting with the Trenums, Gioia was more succinct. He told them Austin’s case was a perfect storm.
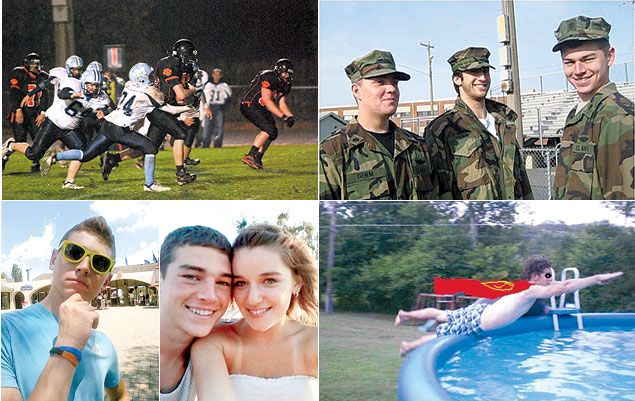
On the first snap of Brentsville’s first football game without
Austin, the school’s quarterback mimed a handoff to his absent fullback, then took a knee. He pointed to the night sky, where cheerleaders with the number 43 painted on their cheeks had released the same number of balloons. The whole school wore white. Cody and Walker wore jerseys bearing their brother’s number, 43, and watched from the sideline. At the end of the game, a Brentsville player carried Walker off the field on his shoulders.
Football went on. The Trenums understood. Gil, 46, had grown up in Ohio and Texas, states where the sport is practically a religion; Michelle, 48, was raised an hour and a half from Odessa, Texas, the real-life setting of Friday Night Lights. She remembers pep rallies and rabid boosters, caravans of cars with shoe-polish-painted windows, what seemed like entire towns turning out for high-school games. Gil and Michelle attended Texas Tech, where Austin went to summer football camp. They loved the sport. So did Cody, a member of the Brentsville High JV squad, and Walker, who played on a youth team.
As the Trenums grieved, friends and neighbors brought them food, mowed and reseeded their lawn, even repainted their front door. The family watched football. Tuesday nights. Thursday nights. All weekend long. College and pro. Tackle after tackle, hit after hit. “I don’t know why,” Gil says. “We just did. It was a distraction, something you had to focus on.”
Gil and Michelle kept in touch with Gioia. They had donated Austin’s brain to the Boston University scientists, who were studying the effects of concussions and head trauma. The Trenums came to a frightening realization: Like so many others around the country, the Prince William County school system wasn’t doing enough to address athletic concussions. What happened to Austin could have happened to anyone.
Six months before Austin’s death, Virginia had passed a law requiring schools to educate students and parents about concussions and to remove students suspected of sustaining the injury from the field of play until cleared by a medical professional. In Fairfax County, education meant watching a ten-minute online video; in Loudoun County, it meant signing a two-page form. Prince William’s policy was still being written, not scheduled to take effect until 2012.
A member of the Prince William County school board, Gil wanted something quicker and better. A policy with teeth. He lobbied administrators. He had Gioia make a presentation to the board, got input from Nowinski, the former Harvard football player now with the Boston University program. Spurred by his son’s death, Gil was
relentless.
Prince William’s new concussion policy went into effect in the summer of 2011, mandating stricter return-to-play guidelines and more thorough education for school athletic trainers. Students trying out for sports are now required to attend an hourlong concussion seminar with at least one parent.
“I have families contacting me all the time, telling me they can’t thank Gil enough,” says Kendra Kielbasa, an advocate for youth-concussion care and the wife of Austin’s former lacrosse coach. Working with Gil to draw up a policy that stresses post-concussion cognitive rest—the kind Austin didn’t know enough to get—Kendra had drawn
on her own experience. Her son, Connor, was concussed after being dropped on his head during a seventh-grade wrestling match. Emergency-room doctors checked Connor for a brain bleed and cleared him to return to school the next day. Three weeks later, with his grades plummeting and his emotions off kilter, he asked his mother if he could lie down.
“Sure,” Kendra said. “Why don’t you go to your room?”
Connor looked around the living room. “I don’t know where it is,” he said. “Can you take me?”
“The hardest part is that people don’t understand—your child looks like he is fine, but he’s not,” Kendra says. “People have to understand that it’s not just a bad headache for a day or two. And it’s not enough to do [concussion education] in the high schools. We have to bring it to the middle and elementary schools.”
Would more education have saved Austin’s life? The Trenums think so.
Last fall, Cody played in a lacrosse tournament in Williamsburg. Michelle was in the stands. A boy from another team was hit hard and concussed. As his parents pulled him off the field, a woman approached. She said she was a nurse. Michelle could overhear their conversation. The boy was dazed, struggling to remember things.
“Well, he’s not passed out,” said the nurse. “That’s a good sign.”
Actually, Michelle thought, episodic amnesia is more of an indicator of serious problems than passing out is.
The nurse continued to offer medical advice, much of it dated. Michelle began to panic. As soon as the nurse left, she ran over to the parents. “Take your son to a doctor,” she implored. “A neurologist. Get him some rest. Keep a close eye on him.”
The parents asked, “Are you a doctor?”
“No,” Michelle said. “But my son died last year after a concussion.”
“That scared them,” she says. “And all I could think was ‘At least your son will live.’ ”
• • •
The brains come here, to a red-brick building in suburban Boston. Each is weighed, photographed, and examined for signs of trauma and disease, then carefully sliced in half. One half goes to the upstairs laboratory, where scientists create tissue samples ten microns thin, chemically stained and mounted on slides for microscopic inspection. The other half is placed in a closet-size, stainless-steel freezer, preserved for future study.
“There are more freezers,” says Victor Alvarez, a researcher at the lab. “We’re always looking for more space.”
Football has a problem. The sport kills too many players. Some slowly, some all at once. The evidence is in the freezers and in the stacks of slides cluttering the office of Ann McKee, a neuropathologist and codirector of the Boston University Center for the Study of Traumatic Encephalopathy.
Each brain tells a story: former Pittsburgh Steelers lineman Justin Strzelczyk, dead at age 36 after leading police on a high-speed chase that began with hallucinations and ended in a fireball; former college-football player Mike Borich, dead at 42 from a drug overdose; former Philadelphia Eagles safety Andre Waters, dead at 44 from shooting
himself; former NFL safety Dave Duerson, dead at 50 from shooting himself in the chest—specifically in the chest—after scrawling a note to his family asking that his brain be donated to science.
Austin Trenum, dead at 17.
Last summer, Gil and Michelle came to McKee’s office. They looked at slides of Austin’s brain. Through the microscope, they saw axons, the long, slender fibers that connect nerve cells and conduct electricity in the brain. In a healthy person, axons run together like fiber-optic cable, straight and smooth. Austin’s were twisted, bulbous,
broken. In scientific language, it was a multifocal axonal injury; in layman’s terms, the equivalent of frayed automobile wiring. Turn on the radio and the windshield wipers might move; turn off the lights and the whole car might shut down.
Michelle choked up. This, she thought, is my baby. This is what ended his life.
Austin’s case isn’t unique, McKee says. There have been other sudden, inexplicable suicides following concussions—some in the military, some among high-school football players. Scientists are struggling to understand the connection. But something is happening. Something terrible.
“It’s the same pattern,” McKee says. “They have disordered thinking and electrical impulses in the brain. They have a minor irritation. And they just want to end it. It’s like having a fly in your room and deciding to blow up your house.”
• • •
A decade ago, McKee wasn’t studying dead football players. Nobody was. That changed when Bennet Omalu, a forensic pathologist and neuropathologist, examined the brains of former Steelers linemen Mike Webster in 2002 and Terry Long in 2005. Both had suffered slow, puzzling descents into erratic behavior and madness, with Long ultimately killing himself by drinking antifreeze and Webster dying of heart failure after an extended period of living in his truck in which he sometimes shot himself with a Taser gun in order to sleep and other times sniffed ammonia to stay awake.
Omalu found that each had suffered from chronic traumatic encephalopathy (CTE), a progressive neurodegenerative disease similar to Alzheimer’s and linked to the absorption of repeated blows to the head, a condition previously associated with prizefighters—in layman’s terms, “punch drunkenness.”
Evidence suggests that CTE is caused not only by concussions but also by subconcussive trauma. Little hits—the ones inherent in football that occur on every snap, like the 1,000 to 1,500 hits to the head that Boston University researchers estimate the average high-school lineman takes each season, some at forces equivalent to or greater than a 25-mile-an-hour car crash.
CTE has been found in a number of deceased football players, including Strzelczyk, Creekmur, Borich, Waters, Duerson, and Chris Henry, a former NFL receiver never diagnosed with a concussion. Early stages of the disease also were discovered in the brain of Owen Thomas, a 21-year-old University of Pennsylvania football captain who hanged himself, and in Nathan Stiles, a 17-year-old high-school player from Kansas who collapsed during a game and died of a rebleed of a brain injury suffered in a previous game.
Because their brains are still developing, children and adolescents are particularly vulnerable to brain trauma. A recent Virginia Tech study measuring head impacts among seven- and eight-year-old football players found that some hits generated more than 80 g’s of force, equal to the blows delivered in college football.
“I think that in ten years we’re going to look back at this and say, ‘Whoa,’ ” says McKee, who has examined thousands of brains over 26 years. “The public only knows some of the evidence. It’s overwhelming. And as it accumulates, it’s impossible to deny.”
• • •
Austin Trenum showed no signs of CTE, none of the telltale clusters of dark brown spots on slides of stained pinkish brain tissue.
The sport damaged his brain nonetheless.
At a 2009 congressional hearing, Ann McKee presented a summary of her work, acknowledging that hundreds of thousands of former football players seem perfectly healthy. She then asked: Do we expect that 100 percent of cigarette smokers will develop lung cancer? Do we expect 100 percent of children who play with matches or even chainsaws will get hurt?
Representative Ted Poe, a Texas Republican, said that parents and players already know football is dangerous. He said government involvement would mean “the end of football as we know it” because the sport would end up becoming “touch football.”
Such are the terms of an ongoing national debate over football’s safety and long-term viability, an argument that has intensified since the May suicide of popular former NFL linebacker Junior Seau. Mismanaged concussions can cause permanent harm and death. But even players who never have a concussion are at risk of developing CTE. How much is too much?
McKee is no abolitionist. She grew up in Wisconsin rooting for the Green Bay Packers. Her favorite player was Willie Wood, a DC native now suffering from dementia. Her two older brothers played the game. She doesn’t want to end football; she wants to save the sport from itself. Three years ago, she ran into a group of players from her daughter’s high school at a doughnut shop outside Boston.
“So,” McKee asked, “you guys know anything about concussions?”
“Oh, yeah,” said one of the boys. “I’ve had five.”
“I’ve had seven,” said another.
“It was a badge of honor,” McKee recalls.
For years, McKee loved attending prep football games. Not anymore, she says. You just don’t know what will happen.
The room remains as it was. A lacrosse helmet. An SAT prep book. A half-empty pack of gum. All on a desk. Austin and his friends mugging in a photo booth, young and happy and full of life, the snapshots tacked to a mirror. Clothes are piled on the closet floor, the bed unmade. Sometimes Michelle will come upstairs and lie down, just to feel her son’s blanket.
Downstairs is a bathroom. When Austin was in the hospital, doctors working to save his life, Michelle tried to make a deal with God: I’ll rip out the bathroom, make it bigger. Austin can be a vegetable and we’ll take care of him. Just let him live.
“But I knew,” she says, her voice trailing off.
The first months were the hardest. Gil, a senior engineer at SAIC, went back to work. The boys were in school. Michelle, a stay-at-home mom, would lie on the living-room couch—the family’s golden retriever, Biscuit, at her feet—and sob. Before Austin’s death, she had been outgoing, involved in the community, digging up local land-use records and political-campaign contributions to lead a successful fight against a planned rock quarry. Not anymore.
She withdrew, felt vulnerable, couldn’t be around people who didn’t know Austin. She threw herself into spy novels, then science fiction, sometimes reading for seven hours a day. She had once favored Anne Tyler and Pat Conroy, selections from Oprah’s book club. “But I couldn’t read those,” Michelle says. “Nothing with mothers and kids and emotions.”
When children take their lives, parents blame themselves. Michelle wondered why she’d gotten on Austin about his homework; Gil wondered why he’d let him do homework in the first place. A grief counselor told Michelle it would take a year for the guilt to pass. “Even I have trouble sleeping sometimes,” says Patti McKay, the Trenums’ close friend. “I think about what Gil and Michelle saw. I don’t know how they sleep. I can’t imagine living with that.”
Michelle still watched football, but not in the same way. She winced at every big hit, noticed that concussed players almost always fell with their forearms extended away from their bodies, a reflex scientists call “the fencing response.” She began investigating sports concussions and teen suicide, spending hours online, reaching out to military and academic experts.
Researchers at the Centers for Disease Control and Prevention tracked suicides, but they didn’t correlate those deaths with recent brain trauma, never mind athletic participation. Nor did anyone else.
Michelle befriended Dustin Fink, an Illinois-based athletic trainer who runs a concussion blog. Fink’s anecdotal evidence suggested that boys who played both linebacker and running back were at greater brain-trauma risk. Michelle made a spreadsheet, one she still maintains, logging every instance she could find of high-school and college football players killing themselves: name, age, position played. She saw a pattern. Linebacker. Running back. Linebacker. Running back. Just like Austin.
• • •
Two football helmets rest on a table. One is black, matte and battered, with an orange mouthpiece wedged in the facemask. The other is reddish and gleaming, decorated with a skull and crossbones and a breast-cancer-awareness sticker. Two gashes run down the front.
The first helmet belonged to Austin. The second belongs to Walker.
Michelle pushes them together. “This,” she says, “is how it happens.”
It’s a Saturday, exactly one year after the weekend of Austin’s death.
Cody finished the previous Brentsville High football season, then quit. He didn’t say why. Walker continued to play for a youth squad, fullback and linebacker, same as Austin. Gil and Michelle didn’t want to overreact, give in to emotion, cocoon their son in bubble wrap. Besides, Austin always took such pride in Walker. The boy loved to hit, so much so that he bragged about it: Mommy, that kid is a baby. He cried, and I didn’t even hit him that hard.
Walker wore a special chin strap, rigged with accelerometers that measured the force of every blow he absorbed. If built-in software deemed any hit powerful enough to cause a head injury, three green LED lights on the chin strap would flash red. While Walker was making a routine block, his head whipped sideways. Red lights. His coach pulled him off the field. Two sideline nurses checked him out. Dizzy and frightened, he cried.
“My head,” he said. “My head.”
The Trenums followed Gioia’s instructions. They made Walker rest. They took him to a Sunday-night bonfire—a memorial for Austin—but didn’t let him run around with his friends. On Monday morning, a neurologist diagnosed Walker with a concussion. Sensitive to light and sound, he was held out of football practice and gym class for a week. One week after that, he was back on the field, Michelle looking on.
“You’re so calm,” one of the other mothers said.
Michelle wasn’t. Watching football on TV was bad enough. This was worse. Also, the chin strap. It was supposed to make things easier, safer. But the lights kept turning red, once when Walker hadn’t even been hit. Michelle made him sit out the entire game. Walker fumed, said he wouldn’t wear the device again. Michelle sent the faulty chin strap back to the manufacturer, got a replacement, then sent that one back, too. More red lights. Was the problem a bad battery? Water leaking into the electronics? Was the problem football?
Michelle wasn’t watching her son. She was watching the lights, waiting for green to go red. She worried about punch-drunk football players, the blows adding up over time—wondered if Walker’s concussion was God’s version of a yellow flag. It was all too much.
Michelle Trenum kept coming back to the same question.
“If you’re that worked up,” she says, “then what are you doing letting your kid out there in the first place?
• • •
Losing a child, Michelle says, is like jumping from one train onto another headed in the opposite direction. In an instant, you’re barreling away from everything you once knew, farther and farther with each second.
Brentsville High has a scholarship in Austin’s name. In their living room, the Trenums keep a large photo of Austin, sweaty and beaming, coming off a football field. On the ceiling above the kitchen table is a spot with his fingerprints, smudged and faded, where he and his brothers once liked to test how high they could jump. “I sometimes think we can never repaint that,” Michelle says. There’s sadness in her eyes—green like Austin’s—and pain.
“I love football,” Gil says. “I loved watching the kids play. But it’s not the same anymore.”
Twelve years ago, Dallas Cowboys quarterback Troy Aikman retired after suffering the tenth concussion of his Hall of Fame career, the result of a vicious hit from Washington Redskins linebacker LaVar Arrington. Aikman since has become a successful broadcaster, a man who owes much to football. After the Super Bowl in February, however, he said that the sport was “at a real crossroads. . . . If I had a ten-year-old boy, I don’t know that I’d be real inclined to encourage him to go play football in light of what we’re learning from head injuries.”
Michelle showed Walker the comment.
“I don’t think I want you to play football,” she said.
He was upset—for a moment.
“Can I play another sport?”
Gil and Michelle are not against football. They don’t judge others. But they’ve made their decision.
“As a mother,” Michelle says, “I’m a lot more relaxed watching basketball.”
Patrick Hruby is a culture writer for the Washington Times and a contributor to ESPN.com and TheAtlantic.com, among others. You can contact him at patrickhruby.net.
This article appears in the August 2012 issue of The Washingtonian.