We’re not saying “subconcussion” anymore. Here’s why.
By Dr. Chris Nowinski, Concussion Legacy Foundation co-founder and CEO
Concussions and sport-related brain trauma have been in the sports headlines for more than a decade. Nearly 1,000 former athletes have now been diagnosed with chronic traumatic encephalopathy (CTE). Most played football, but ice hockey, boxing, rugby, soccer, and other sports have all seen CTE confirmed in former athletes.
But the public and even scientists have struggled to understand why the number of concussions an athlete has suffered does not predict their odds of developing CTE. Many professional athletes I speak to believe they aren’t at risk for CTE because they only had “one or two concussions,” but that couldn’t be further from the truth.
My colleagues and I believe part of the confusion comes from the word we use to describe head impacts and head injuries – subconcussive – so I wrote an editorial with collaborators from Harvard University, Boston University, the Mayo Clinic, and the Concussion Legacy Foundation that was just published in the British Journal of Sports Medicine, the most influential medical journal on sports medicine.
We believe the problem stems from how we think about concussions. We think of concussions as the hardest hits to the head an athlete receives. But when you look more closely at the research, you are reminded that they are not.
We reviewed published helmet sensor studies and found that around 10% of head impacts experienced by football players are harder than the average concussion. Those hits add up quickly. For example, if a football player takes 1,000 head impacts in a season and had one diagnosed concussion, he took around 100 hits harder than that concussion.
But concussions don’t occur every season. A different study of college football players found for every diagnosed concussion, an athlete takes 340 head impacts harder than that concussion. If we want to focus on where CTE risk is coming from, we should not be looking only at the concussions, but at all other hits, and especially those 340 extreme impacts.
We believe the terminology used to describe hits to the head also causes confusion. Scientists have been referring to head impacts that don’t cause concussion symptoms as “subconcussive impacts,” which implies they are less than concussions. This has even led to CTE experts saying CTE is caused by “small, repetitive impacts.” But when it comes to size of the hit, 10% of head impacts are more than concussions. We recommend replacing “subconcussive” with “nonconcussive” to better describe these impacts. After a head impact, a concussion was either diagnosed or it wasn’t.
The term subconcussive has not only confused the discussion around head impacts, but also around traumatic brain injuries. Studies consistently show that athletes exposed to hundreds of repetitive head impacts, in the absence of a concussion, still have changes to brain function, blood biomarkers of brain injury, and structural changes on imaging that look similar to changes in athletes with diagnosed concussions. The concept of subconcussive injury has been shoehorned into the conversation to explain this “missing link.”
We suggest we stop using “subconcussive injury” because it’s also misleading. The missing link is better described as subclinical traumatic brain injury (TBI). Subclinical TBI happens when there are changes in brain function, biomarkers, or imaging without concussion signs or symptoms.
There is no question in my mind that subclinical TBI happens regularly. Beyond the existing studies showing a link, consider this question: the human brain has about 86 billion neurons – if you injured one neuron, could you feel it? Look at the amazing image below, from a new project at Harvard that scanned 1 cubic millimeter of the human brain, to begin to understand the complexity of the human brain.
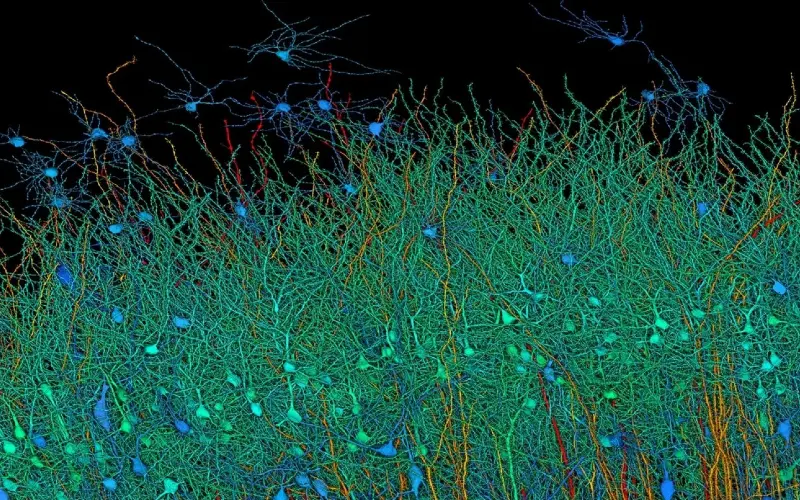
Photo credit: Google
We cannot hear when one tree falls in a forest of 86 billion trees. It is well known that someone can suffer a significant brain injury without signs or symptoms, simply because the injury occurred in an area that is not responsible for common concussion symptoms like memory, thinking, vision, balance, hearing, speech, etc.
By changing the nomenclature, we hope to remove some of the mystery as to why concussions do not predict CTE risk, whereas the number and strength of repeated head impacts do. We need to name the impacts and injuries that we can’t see to advance the conversation.
This is analogous to understanding sun exposure and skin cancer. I was putting sunscreen on my kids recently to prevent them from getting sunburn, which is linked to skin cancer. Sunburn is something I can see. Sunburn is something my kids will complain about because it hurts. Sunburn is analogous to concussion, which we can see and people can feel.
But I recently learned from my travels cofounding the Australian Sports Brain Bank that if I lived in Australia, I would be taught to be worried about how much time my children spend in the sun overall, not just sunburn, because “healthy” sun exposure also causes skin cancer. In Australia, some primary schools have a “No Hat, No Play” policy for children at outdoor recess. Thanks to research, Australians realized they cannot just focus on the shiny objects of sunburns to prevent skin cancer, as overall minutes in the sun matter, too.
To me, that sun exposure is analogous to subclinical TBI. We haven’t cared about it because we can’t see it, and athletes don’t complain about it because they don’t feel it. We also haven’t understood the downstream effects – but now we do. To prevent CTE and other outcomes, we need to focus on preventing subclinical TBI, too.

Photo credit: Just A Little Further
The next time you see that big hit in an NFL game and it makes you hold your breath, you shouldn’t necessarily exhale and celebrate just because the player pops up. They may have suffered a subclinical traumatic brain injury that they cannot feel – but may contribute to developing CTE down the road.
I’m not saying you cannot enjoy watching the game. But I hope you choose to support efforts to limit the number and strength of those impacts – such as the new NFL kickoff, or the elimination of hitting in practice, spearheaded by the late Dartmouth coach Buddy Teevens.
By using the right terms to understand what causes CTE, and letting the science drive changes to how we play sports, we can prevent a lot of cases of CTE.