By Dr. Chris Nowinski, Concussion Legacy Foundation co-founder and CEO
Over the past nine days the sports concussion and chronic traumatic encephalopathy (CTE) community has been rocked by multiple allegations of plagiarism against Professor Paul McCrory, lead author of the 2nd to 5th Consensus Statements on Concussion in Sport, which has led to multiple retractions and a dark cloud hanging over his career and any scholarship he has touched. This blog by Dr. Nick Brown outlines multiple other instances of possible plagiarism by McCrory.
McCrory has been perhaps the most influential voice representing professional sports organizations in their organized efforts to minimize and dismiss the evidence that repeated hits to the head – like those in American and Australian football, soccer, and rugby – can cause CTE. He famously belittled CTE as ”all the carry on and hoo-ha you get from the United States” in a 2016 lecture at the University of Melbourne Florey Neuroscience Institute.
A close view of that 2016 lecture reveals something potentially even more concerning than plagiarism. In his presentation, attended by a VIP audience including former AFL chief executive Ross Oakley and members of the media, McCrory dramatically misrepresented research by Boston University in ways that minimized CTE.
Before I delve into those examples, I’ll provide some background on why McCrory’s statements on CTE matter so much.
Background
The 5th Consensus Statement on Concussion in Sport, published in 2017, is the most influential document of the last decade because of one sentence deep in the document, “A cause-and-effect relationship has not yet been demonstrated between CTE and SRCs (sports-related concussions) or exposure to contact sports.”
Even by 2017, that statement did not align with the views of two of the top U.S. government officials leading CTE research, Dr. Walter Koroshetz, the director of the National Institute of Neurological Disorders and Stroke (NINDS), and Dr. Dan Perl, the head of the CTE brain bank for the U.S. Department of Defense, who both went on record in 2014 saying cause and effect was demonstrated to their satisfaction. From ESPN:
Asked about Goodell’s statement that medical people will decide if there is a link between football and brain damage, Perl said, “I think they have decided. At least some of us have.” Perl acknowledged there may be contributing factors but added: “CTE is only seen in the setting of repeated head trauma. At the end of the day, this is produced by head trauma. I’m sorry, that’s what all the research says.”
Koroshetz, of the NIH, agreed that advanced CTE cases are clearly related to head trauma. “I don’t think there’s any wiggle room,” said Koroshetz, adding that some of the earlier cases may be less certain. “It’s pretty clear this is due to head injury. Whether there are other things involved, and when it starts, that’s hard to know, but I don’t think there’s any question that it’s related to head injury.”
The National Football League went on record in 2016 at a Congressional hearing acknowledging the link.
Organizations like the NHL relied on the consensus statement to claim that causation had not been demonstrated. The NHL was fighting a lawsuit from retired players and regularly cited the consensus statements while defending its inactions.
The Consensus Statement is organized and written by members of the Concussion in Sport Group, and the meeting is sponsored by IOC, Fédération Internationale de Football Association (FIFA), International Federation for Equestrian Sports (FEI), World Rugby (WR) and the International Ice Hockey Federation (IIHF). It has been the subject of exposes from the Canadian Broadcasting Corporation, the Guardian, and the Dutch newspaper NRC because 32 of 36 members had ties to professional sports leagues. 5th annual conference co-chair McCrory, who played a leading role in selecting the members, has advised the Australian Football League, FIFA,and the IOC, has received funding from the NFL, and has served as an expert witness for the NHL.
The Lecture: “The Concussion “Crisis” – Media, Myths and Medicine”
With that background, we’ll now explore how McCrory misrepresented the research of Boston University on CTE at a 2016 lecture at the University of Melbourne Florey Neuroscience Institute, according to their 2015 annual report, he served as a professor and senior researcher,
Example 1: The first time McCrory misrepresents the research from Boston University is at 6:40, where he says,
“And the feared CTE that you’ve heard about… the best guess from the group that is pushing this most strongly says the risk is about 4% of retired athletes get it. The other way of looking at it is that 96% of athletes do not get it. Yet if you read the media, particularly from the United States, you get a very different perspective.
That is not what Boston University said. Here is the passage from which he gets the 4% number:
If one considers the prevalence in deceased professional American football players who died between February 2008 and June 2010, there were 321 known player deaths and the brains of 12 of the 321 underwent postmortem neuropathologic examination at Boston University Center for the Study of Traumatic Encephalopathy (BU CSTE). All 12 examined neuropathologically showed evidence of CTE, suggesting an estimated lifetime prevalence of at least 3.7%. If one assumes that all deceased players who did not come to autopsy did not have CTE and that the amount of head trauma in professional football has remained fairly constant over the past five decades, a prevalence of 3.7% would result. Although this represents a conservative estimate, it suggests a significant public-health risk for persons who suffer repetitive mild traumatic brain injury (TBI).
The passage is meant to infer that even if we found the only 12 cases of CTE among those 321 NFL players, it’s a major public health problem. But the paper also makes it clear that 3.7% is an absolute minimum prevalence, it is unlikely those were the only 12, and it was still statistically possible at that time that 100% of NFL players had CTE. Therefore, when McCrory said that BU said “the risk is 4%,” he is misrepresenting the research.
McCrory made the same claim in a 2013 publication, where he went further, claiming that if our 12 NFL CTE cases (out of 12 brains studied) represented all NFL CTE cases ever, “the incidence rate would be less than 0.01%.”
Journalist Wendy Carlisle was so befuddled by McCrory’s claims that in 2014 she wrote him this letter where she pointed out his misrepresentation and asked, “Why did you think it was methodologically valid to look at all the professional players who were ‘at risk’ i.e.- all those who have ever played professional football and then analyze them against the cohort of autopsied brains of players who died between Feb 2008 and June 2010?”
It’s a great question.
Example 2: The more egregious misrepresentation of the research of Boston University takes place at 31:30, where McCrory says,
“The biggest group in the world pushing this area is the Boston University Group, led by Ann McKee and Bob Cantu, and they’ve presented 64 athletes with “so-called” CTE. But interestingly, a fifth of them had no actual pathology. Yet they’re labeled as CTE. Doesn’t really make sense.”
This is an incredible misrepresentation of a 2013 study I co-authored and that is not what the publication actually says. It is not true that “a fifth of the 64 athletes diagnosed with CTE had no pathology.” Dr. McCrory appears to be referring to this passage on page 60.
We analyzed the brains of 85 individuals with a history of repetitive mild traumatic brain injury and found evidence of CTE in 80%; all males, ranging in age from 17 to 98 years (mean = 59.5 years), including 64 athletes, 21 military veterans (most of whom were also athletes) and one individual who engaged in self-injurious head-banging behavior.
100% of the 64 athletes diagnosed with CTE had CTE. What McCrory does not appear to understand is that throughout the paper we note that most of our Veterans were also athletes, so when we mention athlete and Veteran numbers, some are double counted. It is important for interpreting the data, so the point is raised in the second sentence of the abstract:
We analyzed post-mortem brains obtained from a cohort of 85 subjects with histories of repetitive mild traumatic brain injury and found evidence of chronic traumatic encephalopathy in 68 subjects: all males, ranging in age from 17 to 98 years (mean 59.5 years), including 64 athletes, 21 military veterans (86% of whom were also athletes) and one individual who engaged in self-injurious head banging behavior.
I have never seen anyone make the mistakes that McCrory has made in referencing our studies, including members of the media without medical training, bloggers, or even laypersons on their social media accounts.
These are not the only examples of McCrory misrepresenting the research of others in a way that minimizes CTE. History Professor Stephen Casper has pointed out that McCrory consistently made mistakes in citing the work of others, even making the false claim that Harrison Martland’s seminal 1928 article Punch Drunk was based on the examination of only one patient when it was five.
McCrory also makes an unfathomable error at 19:15 interpreting the number of concussions caused by sports and recreation in America, saying:
Most people think football is the big one but it’s not. In America, where we have the best statistics, the numbers of concussions – sport-related concussion I’m talking about – are probably in the order of 40 million cases a year, if you allow for the unreported cases. If you go on the U.S. Census data it’s probably10 times greater than that again.
McCrory is confused here. He is citing data from a 2006 study from the CDC. But what he doesn’t appear to understand is that the 1.6 to 3.8 million figure on his slide is an extrapolation of a prior CDC estimate of 300,000 sports-related concussions that already accounts for unreported concussions. The CDC provides such a wide estimate (2.2 million!) because they recognize the actual number may be anywhere from five to 12 times higher than their earlier estimate of 300,000.
But McCrory appears to believe the 3.8 million figure is the real number of diagnosed concussions, and then, accounting for undiagnosed concussions, the true figure is 10 times more than that – 40 million concussions. To put it another way, Paul McCrory, the supposed world’s expert, believes that one in eight Americans suffer a concussion each year through sports or recreation.
Then he doubles down yet again and says that U.S. Census data reflects it may be 10 times that number, so Paul McCrory believed, in 2016, after authoring the 2nd, 3rd, and 4th consensus statements on concussion in sport, that there are 400 million sports concussions in America – more than one concussion for every man, woman, and child – each year.
That mistake also provides context for another bizarre statement he makes about our 2013 study, when he says at 32:10: “But as you can see here, 5 (CTE) cases had no symptoms, so that’s a weird disease that doesn’t give you any problems.”
In this statement, Paul McCrory appears completely unaware of a concept widely known in the Alzheimer’s disease field as preclinical Alzheimer’s. Pathology always precedes symptoms in neurodegenerative disease. In Alzheimer’s, it has been shown that most people have pathology 15 years before they show any symptoms. People also develop CTE pathology years before they display symptoms.
Conclusion
Paul McCrory is a complicated man. This 2018 expose by journalist Wendy Carlisle provides even more background, including the discovery that up until that point, McCrory had published no original research on CTE.
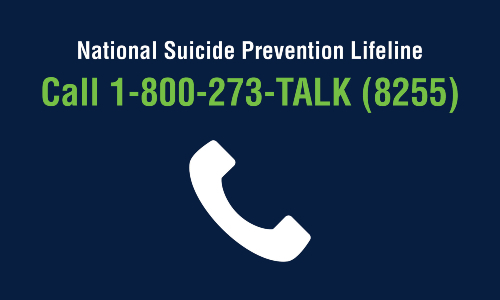
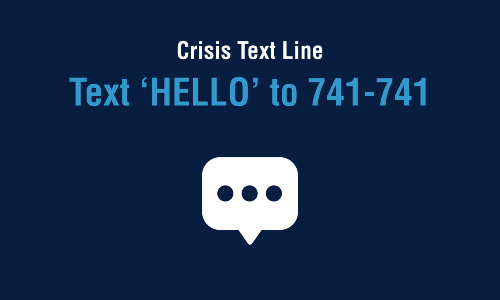
These new revelations of McCrory’s plagiarism, along with the knowledge that he has been misrepresenting the research of others for years, is troubling. People are dying every day of CTE. Families are suffering. It was just announced that CTE was diagnosed in 12 of the first 21 Australian athletes whose brains were studied at the Australian Sports Brain Bank.
Yet many sports minimize the risk of CTE because they’ve been listening to Paul McCrory tell them that CTE is hoo-ha. In my opinion, this is more than just a question of ethics and academic integrity, it has harmed athletes.
Every sports organization that has relied on McCrory’s denial of the link between head trauma and CTE must start fresh. Perhaps they should start with the U.S. Centers for Disease Control and Prevention (CDC) 2019 fact sheet, which states:
The research to-date suggests that CTE is caused in part by repeated traumatic brain injuries, including concussions, and repeated hits to the head, called subconcussive head impacts.
Whatever comes next, the future of the Concussion in Sport Group is in question.
On Friday, McCrory tendered his resignation from the group and will no longer serve as chair. Who will take his place? Consider this – if the next chair says they agree with the CDC and the NFL that head impacts cause CTE, they may cost their sponsors FIFA and World Rugby billions in future payments to injured players.
Therefore, it is only logical to conclude that the sponsors of the Concussion in Sport Group may be forced to select someone not based on their merits as a scientist, but based on their willingness to continue say that “a cause-and-effect relationship has not yet been demonstrated between CTE and SRCs (sports-related concussions) or exposure to contact sports.”
Perhaps this is the time to take a new approach to advancing global concussion and CTE consensus. It is clear the conversation should not be solely driven by the sports industry due to their clear conflicts of interest. Instead, an approach that emphasizes transparency, includes public health expertise, and focuses on the long-term interests of the athletes themselves may prove more valuable. That is precisely the plan laid out by my colleagues in Toward Complete, Candid, and Unbiased International Consensus Statements on Concussion in Sport, published in October of 2021. I encourage you to read it. It is time for change.
*Disclosure: CLF co-founder and chief medical officer Dr. Robert Cantu is a member of the Concussion in Sport Group. He has been publicly critical of their CTE statements.