Mark DeGiovanni
What I Would Tell My Younger Self about Concussions
Ask most young children what sport they want to play, and their answers are probably similar: soccer, basketball, football, baseball. But for Dahlton Brown, it was always wrestling. At just eight-years-old, Dahlton fell in love with the sport. Sure, it may have been a logical choice since Dahlton was big for his age and had exceeded weight restrictions for youth football. He was immediately enamored with wrestling’s competitive nature and the fact he could be an athlete while being a “big kid.”
Dahlton continued to wrestle into the 8th grade; while also losing weight so he could join the football team. He continued participating in both through high school, adamant they were his way forward into adulthood.

Still, wrestling remained Dahlton’s true passion, even after his first diagnosed concussion as a high school sophomore. A mishap during a match knocked him out for several minutes and he had to be rushed to the nearest hospital. He didn’t know it then, but that injury would be classified as a traumatic brain injury (TBI). A neurologist suggested taking some time away from football, due to symptoms he exhibited that included vertigo and balance issues.
Wrestling, however, was fair game. Dahlton was back at it as soon as he cleared, in spite of lingering injuries he sustained from that accident, including sprained C1 and C2 vertebrae, a dislocated shoulder, and a fractured palate. He made it through the season, determined to pursue the sport collegiately.
That dream became a reality when Dahlton attended Stanford University as a walk-on to the wrestling team. He remembers that time fondly and is fortunate to still have close relationships with his former teammates. Balancing his academics with athletics proved to be a challenge and Dahlton chose to step away from the sport to focus on his studies.

Within weeks of leaving wrestling, Dahlton was approached by the Stanford men’s rugby coach during a gym session and asked if he wanted to join the team. After attending one practice, he was hooked.
“I loved rugby’s physicality and camaraderie,” said Dahlton. “And honestly, I was pretty damn good at it.”

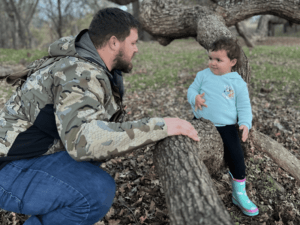
Despite not having played before, Dahlton earned all-conference honors twice. After finishing graduate school, he considered taking a run at semi-pro or even professional rugby. Instead, Dahlton met a woman and chased love instead. It ended up being the perfect choice – they’re now happily married with a beautiful two-year-old daughter, Romie.
Dahlton acknowledges not knowing much about concussions during his youth, other than seeing the movie Concussion with Will Smith. Incidentally, that was also the first time he had heard about Chronic Traumatic Encephalopathy (CTE). While he loved the movie, it didn’t change how he thought about his brain or the sports he played. Dahlton only took brain injuries seriously once he entered college, as there were much stricter return-to-play protocols and more chance for education.

Thinking back on his sports history, Dahlton can recall a couple of concussions so significant they required him to leave during play and either trigger a concussion protocol or keep him out of competition for an extended period of time:
- 2007, high school football when he used forehead for a hard block
- 2009, wrestling – he fell unconscious after an opponent landed with full body weight on Dahlton’s face; left him with a memory gap between warming up for his match and waking up in an ambulance
- 2012, college wrestling practice – he collided with a wall and had to go to the ER for X-rays and other scans
- 2015, college rugby – he was kicked in back of head by an opponent during a tackle
- 2016, college rugby – inadvertent knee to the forehead during a maul
In addition, Dahlton believes he had quite a few undiagnosed concussions – hits to the head that left him stunned, but nothing that caused him serious concern or forced an athletic trainer to stop him from playing.
“Since the professionals never said anything, I just kept going,” said Dahlton.
With each of his concussions, Dahlton experienced varying symptoms; some were short-term for him, such as headaches and sensitivity to light. Others, like vertigo, continue to affect him to this day.
There were also the nonconcussive impacts Dahlton experienced, likely in the hundreds. As an upper weight wrestler, his forehead was considered one of his biggest weapons during competitions. Collisions with opponents were common, as were snapdowns, hand fights, headbutts, and falls to his face. Add in the years of rugby when he played prop, the position most likely to weaponize their forehead, and the number grows even more.

Now at age 31, Dahlton considers himself significantly more educated on concussion, TBI, and CTE, and thinks very differently about them than he had in the past. All aspects of his life have been touched by what he suspects are CTE symptoms, including aggression, mood swings, depression, anxiety, and issues with memory and executive function.
“I wish I knew what I know now, back when I was 16,” said Dahlton. “It would have made a world of difference in my health and my neurological outlook to have taken concussions more seriously.”
In 2017, Dahlton started seeing a therapist for some of his depression and anxiety-related symptoms. He’s also tried nearly a dozen different combinations of antidepressants, stimulants, mood stabilizers, and homeopathic medication. They help keep some of his problems at bay, but he still feels more challenging days than easy ones.
“I’ve spent the last decade or so trying to navigate an ever-changing landscape of mental and physical health symptoms that have escaped adequate treatment,” said Dahlton. “While I’m absolutely guilty of making ‘CTE jokes’ at my own expense, I never took the threat seriously until doing the right research and connecting the dots.”

Dahlton immersed himself in all the literature he could get his hands on to better understand the science. He also reached out to the CLF HelpLine in 2024, receiving personalized resources to help with some of his issues. After reading the stories of fellow athletes and those battling similar issues, he was further moved to take action and support CLF’s mission.
First, Dahlton pledged to donate his brain to advance critical concussion and CTE research in the future. He then joined the Race to End CTE, noting after he first posted about it on Instagram, he had multiple former teammates reach out to express how they’ve been dealing with similar mental health challenges.
“The Race isn’t just about me,” said Dahlton. “At this point, I’ve done my damage and whatever happens, happens. But that doesn’t mean it should continue. As I look at social media with youth sports and the emphasis on early athletic development, I can’t help but worry about my own daughter, who has changed my world in countless ways since she was born. I race for her, and all the other youth of this world, to have agency over their health.”
Dahlton is sharing his story to help others dealing with the aftereffects of concussion and so other parents understand the long-term potential consequences of repeated head trauma.
“Don’t be afraid to talk to someone, especially when it comes to former teammates or your loved ones,” said Dahlton. “Be honest about how you’re feeling and your concerns. While they may not have the exact same experience, it may help to hear their perspective.”
Dahlton knows finding a cure for CTE may be close, and even the ability to diagnose and treat it during life would bring a significant sense of relief. Though he and those around him are aware he’s not an angry or hurtful person at heart, he fears his brain will eventually betray him down the line. For now, Dahlton knows research is the key so we can better understand how to help those battling suspected CTE, and so loved ones can learn about the best ways to provide support during their journey.
Steve Schmitz
Beginnings
I first met Steve in 1972, at the age of 17. He participated in many sports, including football, basketball, baseball, and even golf. He didn’t just play; he excelled. His athletic achievements were featured regularly in local newspapers, so much so he couldn’t go out to places as people would recognize him. It felt like a burden to Steve at times, who certainly loved sports but didn’t want that to define who he was.
While sports took up most of Steve’s life, he was able to keep it separate from everything else once off the field. He preferred spending time with his loved ones, including family, friends, and, of course, me. He was sentimental about the world and thought there was more to him than all that media hype.
Still, Steve’s talent in football was apparent. Colleges were lining up to recruit him and get him to commit. I felt like this process made him lose some of his ambitions and other dreams. Steve once told me he’d like to have been a psychologist or therapist of some kind. I always used to say he could psychoanalyze a telephone pole. Nevertheless, Steve ended up choosing the University of Notre Dame.
Before Steve left for school, we became happily engaged and I decided to stay in Cleveland to pursue a few passions of my own. Since I was pretty active myself, I wanted to become a personal trainer or sports therapist to help others. I think I had a good understanding of safety and always cringed when I saw big head hits in football. Even back then, I felt this was so unhealthy, but that’s just how they were taught by coaches. Athletes had no idea what would happen to them in the future. Of course, we are now starting to see the repercussions of all that damage.
After graduating, Steve was invited to training camp with the Cleveland Browns, going there about one month after we got married. For reasons unknown to me, he ended up quitting and returning home. He said he just wanted to move forward with his life. Taking on various jobs at first, it took Steve a while to find his place in the business world, eventually settling into the moving and storage transportation industry. He was a very hard worker but never brought work home with him.
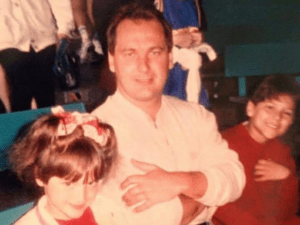
Steve was a wonderful husband and father who prioritized spending time with family. He was patient, compassionate, and always encouraged our children to follow their dreams. Our kids tried various sports with quite a bit of success, while Steve stayed active through local baseball and basketball leagues. It was a busy but fulfilling life.
A Different Steve
As the years went on, Steve started having trouble making decisions and handling our personal finances. He had issues with memory, became confused often, and couldn’t focus. More and more, I had to take over all our family duties.
Steve then had to change jobs several times as he was having difficulties functioning in an office setting. Eventually, he could no longer work. His mind was failing him.
Our kids were now adults and confused by what was happening with their father. I had no answer, as I didn’t understand it, either. The wonderful man I used to know was slowly slipping away. Steve wasn’t the same; he was losing his place, his purpose.
I took Steve to various doctors and neurologists, but even they had no explanation. His health declined to the point where I could no longer leave him alone. I was also working part-time so it was difficult balancing all these responsibilities. Eventually, we lost everything. We used up our savings and retirement accounts to pay for the pile of medical bills and living expenses. Our home and cars went to the banks. We were only able to survive with the help of family, friends, and charities.
But the biggest loss of all was Steve.
My Lost Gladiator
Steve’s spirit was no longer connected to him, and his mind continued to deteriorate. We took many, many trips to different psychiatric centers in the hope any kind of treatment or medication could help Steve. He said he was “afraid of the demons coming after him.”
I had to take preventative measures around the entire house to keep Steve safe from himself and the monsters in his head. He couldn’t tell if something was food or it wasn’t and tried to claw his way into everything. The cupboards, drawers, and closets were locked up. I couldn’t let him out of my sight for a minute. Steve was homebound, a prisoner in his head and in his own home.
In the end, Steve wasn’t going to face these final days without all the love and care we could provide. While I couldn’t connect with him on the outside, I sensed his soul was still in there somewhere. We lost Steve on February 13, 2015, his beautiful spirit going up to heaven.
After his passing, we made the decision to donate Steve’s brain to the UNITE Brain Bank for research. It was undoubtedly the hardest thing I’ve ever done.
I have always felt football is a gladiator sport. Today, I picture Steve in his football uniform standing atop a hill, covered in gladiator armor. From the outside, he seems big, strong, and powerful. But when you look closely, there’s no face – it’s simply blank, like the final years of his life. When he was Steve, he was an angel on earth. Now, he’s an angel in the sky. I always wished I could save him, but God did it first.
It doesn’t get any better than that.