By Chris Nowinski, PhD and Robert Cantu, MD
We are devastated by the tragic shooting in Manhattan in which four people were killed and another injured. The alleged shooter, Shane Tamura, was a former high school football player who died by suicide and left a note saying he believed he had CTE. It has since been reported that in the last few years he had twice been in involuntary psychiatric holds and that antipsychotic medications were found at his home. Teammates have reported remembering Tamura missed practices and games due to at least one concussion.
His brain is being studied by the New York City Medical Examiner, but the findings will not explain the tragedy nor answer all our questions. Despite what he wrote, science cannot answer if Tamura’s psychiatric illness was related to his football career or CTE, if it is even present. Research-to-date suggests CTE will not be present, as among 45 former high school football players studied at the UNITE Brain Bank at the Boston University CTE Center who have died before age 30, 31% have had CTE.
However, we should not overlook the concussions Tamura may have suffered on the football field. We’ve long known that a concussion, also known as a traumatic brain injury (TBI), can cause headaches, memory problems, and sleep disturbances. But what’s often overlooked is how brain trauma, especially when it happens early in life, can significantly increase the risk for serious psychiatric illnesses like schizophrenia and bipolar disorder.
We were both part of a review of how concussion can impact normal brain development in 2011 led by Dr. Dan Daneshvar. That same year, a systematic review by Molloy et al. showed TBI was associated with a 65% increased risk of later psychiatric hospitalization for schizophrenia. Since then, even the link between concussion and psychiatric disorders has only strengthened.
A landmark 2014 study published in The American Journal of Psychiatry analyzed more than 1.1 million individuals in Sweden and found that compared to those without a TBI history, those with TBI were 65% more likely to develop schizophrenia, 28% more likely to develop bipolar disorder, and 439% more likely to receive a diagnosis of “organic mental disorder,” or what is now considered a neurocognitive disorder caused by an external event – TBI, brain disease, infection, toxic exposure, etc. (Fazel et al., 2014)
Receiving the TBI between the ages of 11-15 conveyed increased risk for schizophrenia (86%) and bipolar disorder (30%). These risks were even higher for people with multiple injuries or more severe TBIs, and the associations remained significant even after adjusting for shared familial and environmental factors.
A 2024 study reinforced this connection in children. Sariaslan et al. examined data on individuals born in Sweden between 1973 and 1997 and found that men diagnosed with mild TBI had a 28% increased risk of later developing schizophrenia spectrum disorders, and 59% higher risk for bipolar disorder.
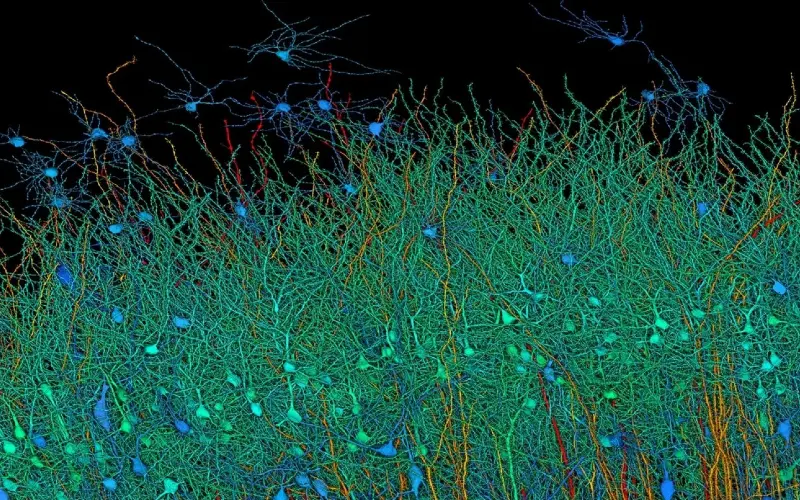
What’s happening inside the brain to cause this connection? TBI triggers widespread neuroinflammation, damages white matter tracts and small blood vessels, and disrupts frontal and temporal lobe function — regions critical for regulating mood, impulse control, and perception. The result is a biological cascade that can prime the brain for long-term dysfunction, especially when the brain injury occurs during adolescence.
In individuals with a family history of psychiatric illness and therefore already at high risk, a concussion appears to sometimes wake a dormant disorder. But psychiatric disorders are also seen after concussion with no family history or risk factors.
We must stop seeing brain injuries, especially in children, only as short-term inconveniences. Every concussion is a potential inflection point in a person’s mental health trajectory. Coaches, parents, and clinicians must take concussion seriously, monitor long-term behavioral changes, and implement early interventions when psychiatric symptoms emerge.
The mental health crisis isn’t just about trauma, stress, or biology, it’s also about unrecognized brain injuries fueling the fire. And unless we confront that reality, we’re going to keep missing the people who need us most.